HFpEF
Symptoms of HF and elevated filling pressures at rest or with exercise, with LVEF >50%
How common?
Lifetime risk may be estimated from (CHS and MESA studies) to be >10% in those age >45.
HFpEF hospitalisations - women to men = 2:1
May be the dominant HF subtype in the future
Prevalence increases with
age
hypertension
obesity
diabetes
Pathophysiology - stiff heart
Hypertension -> myocardial fibrosis -> stiff heart
Obesity -> higher blood volume -> hypertrophy and fibrosis -> stiff heart
Microvascular inflammation (diabetes, obesity, CLD, hypertension) -> microvascular endothelial dysfunction -> reduced NO bioavailability, cGMP, protein kinase G activity in cardiomyocytes -> fibrosis -> stiff heart
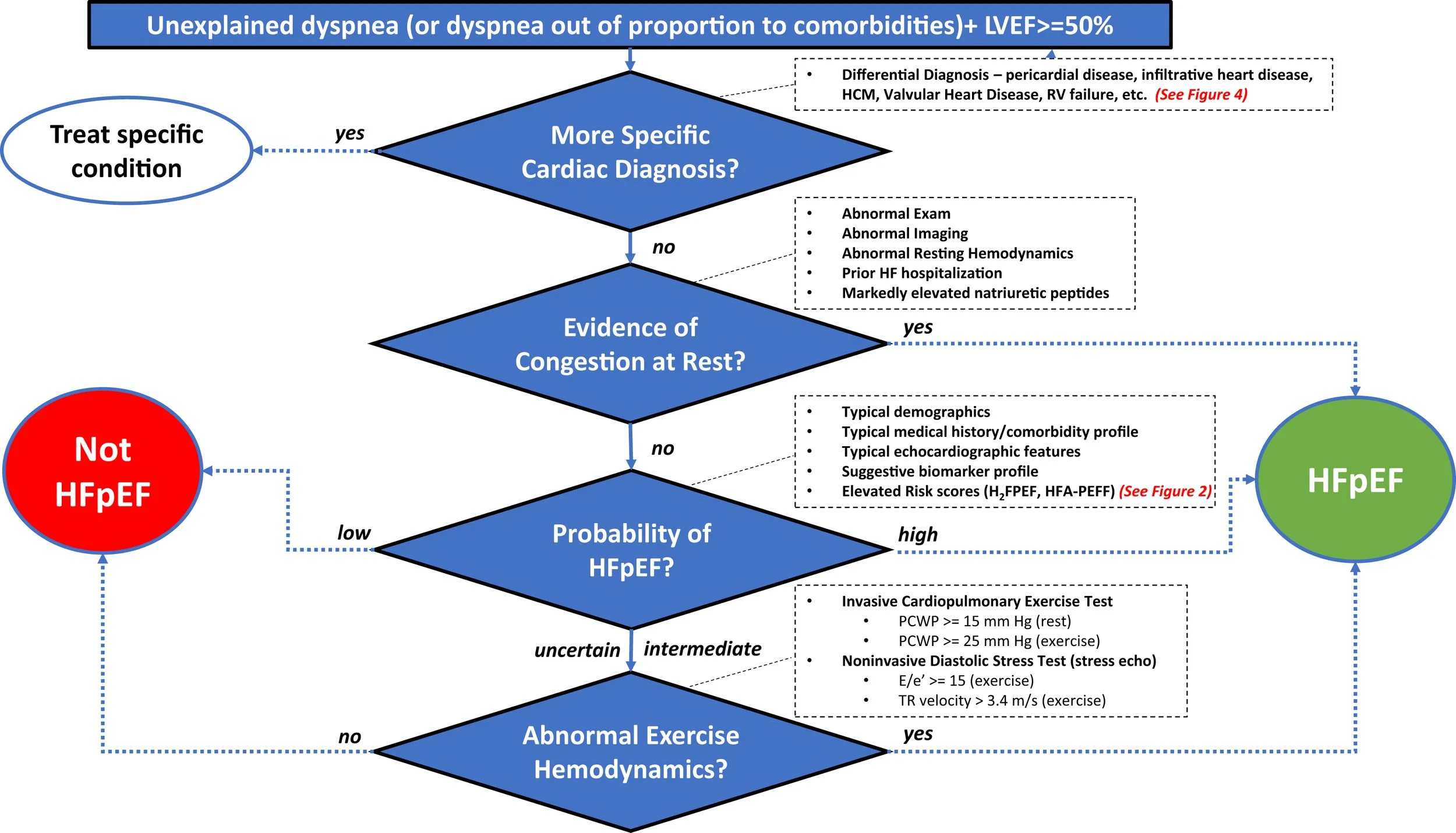
Suggested diagnostic algorithm for HFpEF
Suspect HFpEF if symptoms of HF and risk factors present
Symptoms: dyspnoea, orthopnoea, fatigue, exercise intolerance
Signs: elevated JVP, oedema, pulmonary crackles
Often triggered by infection, AF, uncontrolled BP
Exclude other causes: lung disease, anaemia, obesity alone
Key investigations
ECG – AF, LVH, ischaemia
Bloods – BNP, renal, thyroid
Echo – EF ≥ 50%, LVH, LA size, diastolic parameters
CXR – pulmonary congestion
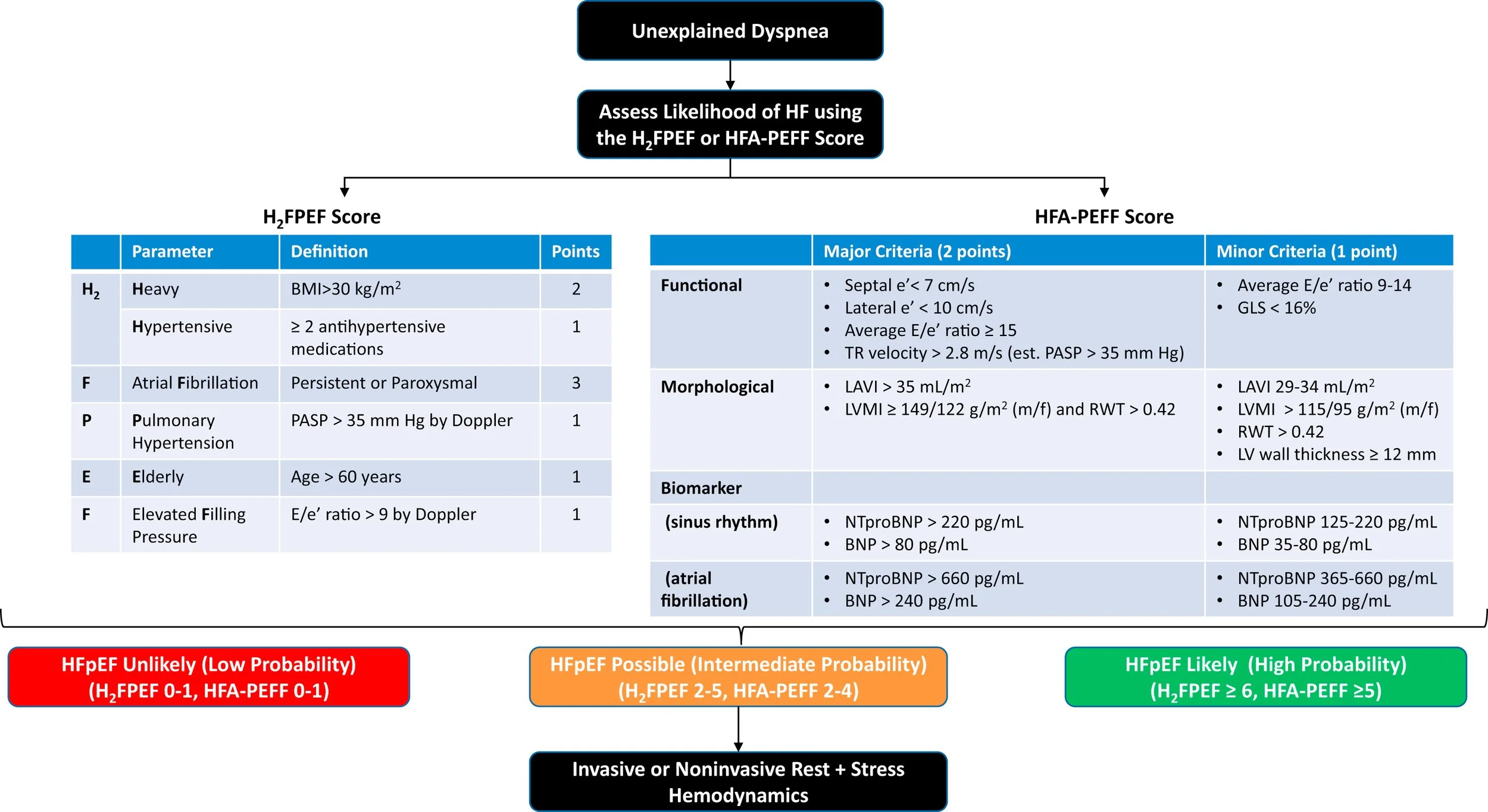
Multiparameters scores may be useful to highlight the important factors to consider: (https://www.jacc.org/doi/full/10.1016/j.jchf.2023.03.011)
Management
Address comorbidities
Obesity
>80% HFpEF pts are obese
Dietary intervention / bariatric surgery associated with favourable outcomes
Awaiting data from trials of weight lose drugs (GLP-1 agonists)
HTN
Consensus guidelines recommend <130/80mmHg
Diabetes
CAD
AF
There may be a role for rhythm control with drugs or CA in the HFpEF population (limited data)
Exercise
improves aerobic capacity and QOL
moderate intensity likely equivalent to higher intensities
SGLT2 inhibitors
EMPOROR-Preserved trial: 5,998 pts, empagliflozin vs placebo in HFpEF. 21% reduction in rates of primary composite outcome of CV death or HF.
DELIVER trial: 6,263 pts, Dapagliflozin vs placebo in HFpEF. 18% reduction in the primary composite outcome.
ACEi / ARNI
In HFpEF generally no clinically important reductions in cardiovascular death or HF hospitalization
MRA
Spironolactone can be considered to reduce HF hospitalization in selected HFpEF patients especially those with LVEF closer to 50%; but caution re hyperK and worsened renal function
Key summary
HFpEF = HF symptoms +/- ↑BNP + preserved LVEF + diastolic impairment.
Common in older, hypertensive, AF patients
Early recognition and treatment reduces hospitalisations.
Treat HF symptoms with diuretic, manage comorbidities, control BP and encourage physical activity.
All patients with symptomatic HFpEF should be treated with SGLT2i (if no contraindications).
Consider withdrawal of beta blockers in patients without compelling indication, substitute with ARB/ACEi (ARNI not subsidized in NZ….) for HTN.
Dr Gary Lau